Sidebar
Research News
Decolonizing Global Health : Know Your Organizational Weaknesses
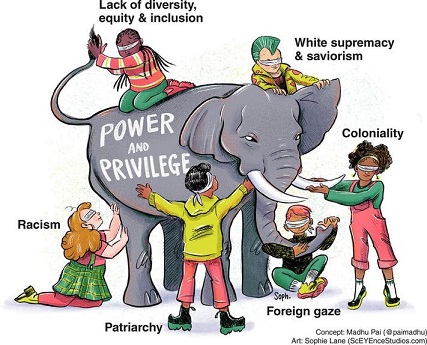 In an interesting interview for Global Health Now (GHN), Carel IJsselmuiden and James Lavery share their view on "how the RFI speaks to the need for organizations to reflect and take stock of any shortcomings". The RFI isn’t a report card that brands institutions as good or bad. It’s intended, instead, to provide a pathway to self-improvement—which is the essence of decolonization.
In an interesting interview for Global Health Now (GHN), Carel IJsselmuiden and James Lavery share their view on "how the RFI speaks to the need for organizations to reflect and take stock of any shortcomings". The RFI isn’t a report card that brands institutions as good or bad. It’s intended, instead, to provide a pathway to self-improvement—which is the essence of decolonization.
(Ref: Joanne Silberner for Global Health NOW)
Find out if you're a Colonizer or Decolonizer
[Announcement:]: Free Mini Certificate in Health Research Ethics for Students

Free ethics training for students in health research ethics!
The 12-hour virtual training is very interactive and features more than 20 experts in bioethics from the APRU network. This year it will take place on April 14/15, April 28/29, and May 13/14.
Space is limited and the deadline to register is April 10, 2022.
‘Working relationships’ across difference - a realist review of community engagement with malaria research
Abstract
Background: Community engagement (CE) is increasingly accepted as a critical aspect of health research, because of its potential to make research more ethical, relevant and well implemented. While CE activities linked to health research have proliferated in Low and Middle Income Countries (LMICs), and are increasingly described in published literature, there is a lack of conceptual clarity around how engagement is understood to ‘work’, and the aims and purposes of engagement are varied and often not made explicit. Ultimately, the evidence base for engagement remains underdeveloped.
Methods: To develop explanations for how and why CE with health research contributes to the pattern of outcomes observed in published literature, we conducted a realist review of CE with malaria research – a theory driven approach to evidence synthesis.
Results: We found that community engagement relies on the development of provisional ‘working relationships’ across differences, primarily of wealth, power and culture. These relationships are rooted in interactions that are experienced as relatively responsive and respectful, and that bring tangible research related benefits. Contextual factors affecting development of working relationships include the facilitating influence of research organisation commitment to and resources for engagement, and constraining factors linked to the prevailing ‘dominant health research paradigm context’, such as: differences of wealth and power between research centres and local populations and health systems; histories of colonialism and vertical health interventions; and external funding and control of health research.
R&D : More Than Sharing Vaccines
"This pandemic is not over until it is over everywhere."
A commentary by COHRED's Executive Director, Board members, associates and partners published in Think Global Health highlights a complete change is needed in the approach to and funding of global preparedness.
Regardless of an increasing provision of vaccines, there are many of the poorest countries, health and research and development (R&D) systems are absolutely lacking to serve the needs of their populations. Although some are privileged to live in countries with effective health research and development systems that can ramp up their responses to such emergencies, many are not. This R&D inequity lies at the core of current and future lost lives.
The COVID-19 pandemic underlines the vaccine inequity is ethically wrong. Its continuation for more than two years into the pandemic shows the limits of global solidarity as an effective global public health strategy. For several decades, most LMICs have invested low in their own R&D ecosystems and remain depended on the scientific, and financing efforts of high-income countries to address their R&D requirements which does not solve the long-term problem of inequitable participation in effective R&D and resulting interventions.
The two biggest current threats to global health security—pandemics and climate change—require equitable access to R&D and implementation.
"Vaccine inequity" should not become "vaccination inequity."
R&D equity should become an explicit objective in national and international development and collaboration policy, especially between high- and low- and middle-income countries.
Mental health and well-being of children in the Philippine setting during the COVID-19 pandemic
Abstract
The coronavirus disease 2019 (COVID-19) pandemic has subjected the mental health and well-being of Filipino children under drastic conditions. While children are more vulnerable to these detriments, there remains the absence of unified and comprehensive strategies in mitigating the deterioration of the mental health of Filipino children. Existing interventions focus on more general solutions that fail to acknowledge the circumstances that a Filipino child is subjected under. Moreover, these strategies also fail to address the multilayered issues faced by a lower-middle-income country, such as the Philippines. As the mental well-being of Filipino children continues to be neglected, a subsequent and enduring mental health epidemic can only be expected for years to come.
Keywords: Mental Health, Philippines, COVID-19, Psychology, Child, Child care, Health services, Social problems












